3 Ways Healthcare Can Be Better, Even After COVID19

Learn from the experts how healthcare, which is traditionally behind the times, can get a sorely needed boost in the wake of the pandemic.
By A.J. Hanna, Sykes Enterprises, & Michael Grace, RPI Consultants
The COVID-19 pandemic has stressed all parts of the healthcare system. And while we are seeing the best f our caregivers and those serving in our communities, we are also seeing more clearly the long-standing barriers to efficient execution of healthcare. Many of these are not simple to fix. Will the American healthcare system take this opportunity to push for change once we have stabilized from the current crisis?
With more than 45 years healthcare experience between the two of us – working for providers and payors, both in operations and IT- we have had front row seats as the American healthcare system has struggled to “keep up with the times.” We have seen how some deep-seated practices are keep the industry from taking advantage of all the modern technology has to offer.
The continual breakdown of interoperability between systems, an understandable but crippling conservatism regarding data security, reluctance to invest in technology, and resistance to administrative change are just some of the obstacles keeping healthcare from moving forward. But COVID-19 has put us in a unique situation; it’s forced our hand and jump-started the overwhelming process of change for the healthcare industry.
Specifically, we see three high-value areas that the pandemic has revealed where improvements would make operations more efficient and enable the industry to respond more effectively in the future: interoperability, data security, and digital transformation.
1. The Case to Improve Interoperability
In the healthcare industry, interoperability is complex. Disparate computer and software systems need to exchange and share data from a range of vital sources, including laboratories, clinics, pharmacies, hospitals, and medical practices. This is no easy task, given that various practices use hundreds of software platforms to document care.
Healthcare has struggled with this for almost a decade and has made minimal progress. The best results come from providers leveraging the same system. The most recent improvement efforts have seen acute-care providers give the post-acute community access to their electronic health record (EHR) systems (Cerner, Epic, etc.), to facilitate easier transfer of information between caregivers.
The benefit to the patient in resolving interoperability issues would be monumental and include better efficiency, safer care, and lower costs.
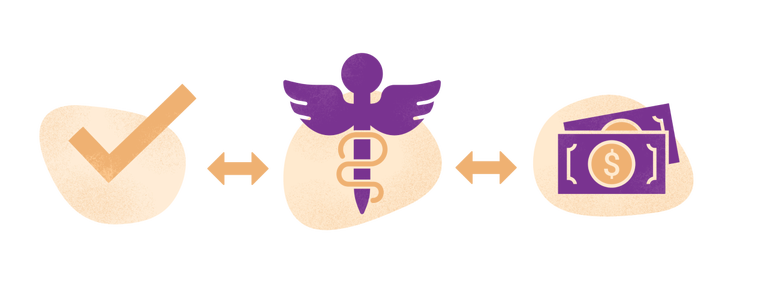
3 Benefits of Solving Interoperability Hurdles
Improved Efficiency
Information should follow the patient and be available to all providers, public health officials, and payors. Imagine the downtick in administrative issues without duplicative patient information entries or medical record transfer delays when a COVID patient moves from an emergency hospital stay to a rehabilitation setting and then to their primary caregivers. With improved interoperability, access to the patient’s information would be immediate instead of potentially delayed by days or weeks to make a full transfer.
Better, Safer Care
With easier access to more information from other providers, doctors could diagnose and treat patients more efficiently and effectively. Often, when patients hear, “We’ll get back to you with the results in two or three days,” much of that is simply the inefficiency of transmitting results between providers. Improved interoperability and even certain advances technologies could serve to provide more reliable patient data and close the gap on receiving critical diagnostic information.
Saved Time & Money
Unnecessary duplicate tests and incorrect procedures are costly, but they could be prevented if data could flow freely and quickly. With immediate, seamless, and free access to full patient medical records, referrals, and medication lists, patients and providers alike would save the time and expense of gathering and moving data between points of care. With more complete and readily available information, it would likewise improve cost-effectiveness for insurance providers in considering claims.
Not only would improving interoperability make healthcare providers’ lives easier while also benefiting their patients, it would allow public health officials to access the flow of data and care information for better prediction of and response to major health events. If we had access to this information at the onset of the pandemic in America, coupled with the appropriate monitoring, we might have been act earlier and proactively allocate resources to predicted high-impact areas.
The resolution to the interoperability issues will no doubt be complex and require a huge investment in resources. However, the changing culture may force the industry to start addressing interoperability now. As it stands, there is a major gap in interoperability. Patient, provider, , and insurance information should flow seamlessly, simultaneously ensuring accuracy, cost-effectiveness, and a higher level of care.
Healthcare organizations that take the lead in resolving the issue will attract those patients who reject old methods of passing information between players they feel are all part of the same care experience. Providers who assure that the software they use complies with standards like the Fair Healthcare Interoperability Resource (FHIR) standard will be in prime position to capture this part of the market.
2. Treat Data Security as an Opportunity, Not an Obstacle
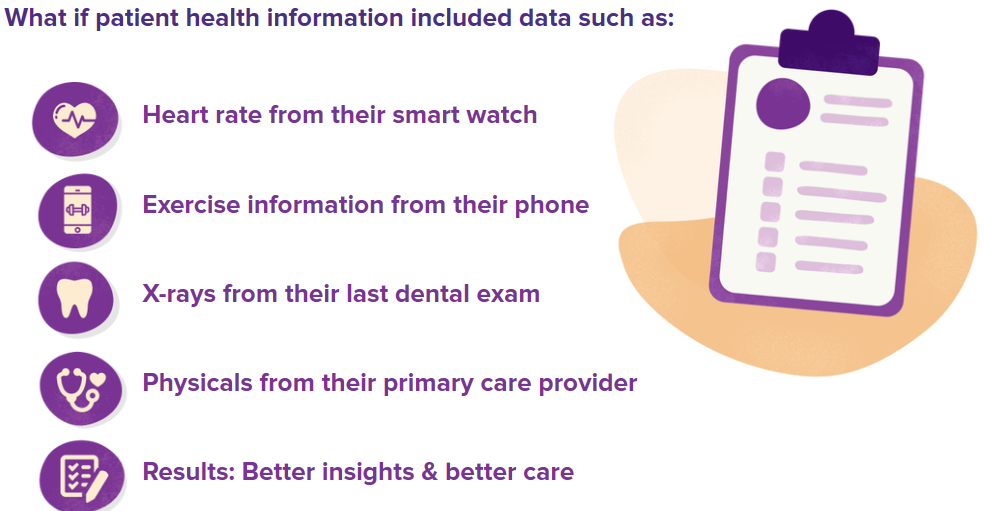
The healthcare industry needs to protect patient data as it embraces more and more digital health technologies, including wearables, diagnostic equipment, telemedicine tools, mobile care apps, cloud applications, and data-driven software platforms. While technology can increase patient accessibility and satisfaction with their overall care, these digital tools don’t come with risks – most specifically to sensitive patient data.
Healthcare information security continues to be a growing concern. An Experian report found that hospital networks continue to be “a ripe target for attackers,” since data is spread over different networks, making it harder to defend than more centralized organizations. (1)
Additionally, the interest in securing healthcare often creates innovation inhibitors. The most secure application is one that exists in a silo and shares no information with anyone or anything. Legacy information security teams used to simply deny access or integration requests, citing them as “a data security risk.” For healthcare to move forward, data security must balance protecting systems, information, and privacy with innovation and interoperability across other systems and organizations.
Data security should become an environment of listening to the needs of the patient and customer and innovating how to secure the data for their requests. This is a paradigm shift that has only just begun with the new guard in information security. Data security professionals must face the challenge of giving users secure access. As consumers want more of their data, and as we have a larger need for access to healthcare data at a global level during a pandemic, this shift is key to predictive analytics and treatments, early warnings of global health issues, and better follow-up care for patients.
Part of the issue comes in finding standards. There are more than 125 healthcare information security companies with as many solutions. Organizations such as Healthcare Information and Management Systems (HIMSS) and HITRUST have struggled to get wide adoption of tools and standards. Organizations typically have their own plan, and some find that moving applications to the cloud provides an extra security layer versus having servers in a hospital data center. While this solves one problem, it can create another related to access to data in the hands of the end users trying to automate processes and create efficiencies. This area of healthcare IT is rapidly evolving, with tools allowing hybrid environments where cloud data can be accessed from on-premises application.
The rapid rate of innovation in information security makes it one of the fastest evolving areas of healthcare IT. Every day, those in healthcare IT are challenged by wearables, new cloud applications, or better access to data. How they respond to these will determine how fast as organization moves along the innovation continuum.
3. Embrace Digital Across the System
Given the challenges with interoperability and the continued focus on data security, it may not be surprising that healthcare lags behind other industries in the adoption of digital technology. Healthcare providers spend significant resources every year in assuring the security of data, maintaining a library of niche applications, and supporting multiple versions of core systems or duplicative systems due to the expense and operational challenges involved in standardizing them. Those factors, along with resistance by clinical staff to changes that might affect the way they spend their time, help to explain why the healthcare industry has historically been a decade or more behind other industries in making technological change.
Cost considerations are certainly in play in many of the areas where technology has been implemented. It’s expensive to install electronic claims and billing systems, electronic healthcare records (EHRs), enterprise resource planning (ERP) systems, and other types of digital tools that other industry verticals have long since implemented and, in some cases, moved on to the next, often cloud-based versions. In many cases, such as with EHRs, regulation has been needed to drive the adoption of technology.
The struggle with user-friendliness happens not only on the back end, but in the way healthcare providers interact with their patients/customers. Retail and consumer-product companies have entered the healthcare market and have been more progressive in their focus on focus on the user experience, forcing healthcare systems to rethink the way they interact digitally with their patients/customers. Driven by a more technology-savvy populace, more healthcare institutions need to advance their ability to seamlessly provide things like online appointment scheduling, pricing and cost research, and access to personal medical information.
It will certainly take a willingness to challenge and change the issues with interoperability and data security to make this happen. And it is time, perhaps, for the creation of a “chief experience officer” in healthcare to focus solely on how to better meet the growing needs and expectations of a world looking for an Amazon-like experience in every interaction.
Moving Forward
The issues presented here are not new, but they need to be addressed faster than the speed of regulation. How much easier would tracking, managing, and sharing information about patients — even between caregivers — have been if these issues had already been addressed prior to the COVID-19 pandemic?
The broader healthcare industry, including regulators, payors, providers, and others, must look at the lessons learned during the pandemic to chart the path for the future. Telehealth, which has spent decades trying to find its place in health delivery, has exploded with the temporary relaxation of regulations, increase in reimbursement, and better accessibility to connectivity. The recent extension and push to make permanent many of the relaxed standards for Medicare coverage of telehealth is a positive step in that direction.
Perhaps as challenging as any other aspect will be the cultural change needed to move forward. A 2019 report from TigerConnect found that 90% of the 200 respondents to their survey in the healthcare sector still rely on fax machines as a primary mode of communication. (2) While healthcare has continued to expand its usage of advanced technologies like machine learning (with mixed results), it is still a culture not wanting to “rock the boat,” especially for clinical staff.
Healthcare must battle the culture of saying “no” to new ideas in the name of security without finding a way to say “yes” to something that solves a problem at hand. And as more people use technologies like telehealth, they will demand even more in the areas of ease-of-use, immediate access, and customer-friendly online tools for their healthcare needs.
Follow us online for faster access to announcements, knowledge base updates, and upcoming events!





